Vaginal Candida: A Global Epidemic, Root Causes, and Probiotic Solutions
Introduction: A Silent Epidemic Affecting Millions
Vaginal Candida, commonly known as a yeast infection, is one of the most prevalent and misunderstood health issues affecting women across the globe. According to the Centers for Disease Control and Prevention (CDC), approximately 75% of women will experience at least one Candida infection in their lifetime, and nearly 40-45% will experience two or more recurrences.
This condition, while not usually life-threatening, profoundly impacts quality of life, intimacy, self-confidence, and mental health. The discomfort, shame, and confusion around vaginal infections make many women suffer in silence—often misdiagnosed, mistreated, or misunderstood.
But what causes this overgrowth of Candida in the first place? Why is it becoming increasingly common in modern societies? And how can probiotics help restore balance naturally?
Let’s explore the root causes, modern lifestyle factors, conventional treatments, and how targeted probiotic therapy, like Akkermansia muciniphila and Clostridium butyricum, may offer a sustainable solution.
Chapter 1: Understanding Candida Albicans
What is Candida?
Candida is a genus of yeast, with Candida albicans being the most common species responsible for vaginal yeast infections. It is usually present in small amounts in the vaginal microbiota, gastrointestinal tract, and skin.
Why does it become a problem?
Under normal circumstances, Candida coexists in harmony with beneficial bacteria, such as Lactobacillus, in the vagina. These bacteria produce lactic acid, hydrogen peroxide, and other substances that inhibit the growth of fungi. However, when this balance is disrupted, Candida albicans transforms from a harmless yeast into an aggressive, invasive fungus.
The Role of Biofilms
Candida forms a protective structure called a biofilm, which shields it from antifungal treatments and immune attacks. This is one reason why standard treatments often fail to provide lasting relief.
Chapter 2: Global Burden of Vaginal Candida Infections
According to a global review published in The Lancet Infectious Diseases, over 138 million women suffer from recurrent vulvovaginal candidiasis (RVVC) annually. This makes it one of the top causes of gynecological visits worldwide.
-
Developed countries see a high incidence due to antibiotic use, hormonal contraceptives, and high-sugar diets.
-
Developing countries report increasing rates due to poor hygiene practices, malnutrition, and limited access to healthcare.
Economic and Social Cost:
Besides the physical discomfort, women spend billions of dollars globally on antifungal creams, prescriptions, doctor visits, and hygiene products.
Impact on Mental Health:
Recurrent infections are linked with depression, anxiety, and sexual dysfunction. Many women report a lack of confidence in their bodies and constant fear of intimacy.
Chapter 3: Key Causes of Vaginal Candida Overgrowth
1. Antibiotic Use
Broad-spectrum antibiotics kill not only harmful bacteria but also the beneficial vaginal flora—particularly Lactobacillus strains. With these defenders gone, Candida flourishes.
2. High Sugar Diets
Candida thrives on sugar. Diets rich in refined carbohydrates, sugary drinks, processed foods, and alcohol create the perfect environment for yeast overgrowth.
Studies have shown that glucose directly fuels Candida’s biofilm formation, making it harder to treat and more resistant to medications.
3. Hormonal Changes
-
Estrogen-rich states like pregnancy, oral contraceptive use, or hormone replacement therapy can enhance Candida adhesion to vaginal cells.
-
Estrogen also increases glycogen in vaginal tissues, indirectly fueling yeast growth.
4. Weakened Immunity
Women with diabetes, HIV/AIDS, cancer, or autoimmune diseases are more vulnerable due to a weakened immune response to fungal pathogens.
5. Poor Hygiene or Overwashing
Using harsh soaps, douches, or scented hygiene products can disrupt the pH balance and kill beneficial bacteria.
6. Tight or Non-Breathable Clothing
Candida loves warm, moist environments. Wearing tight leggings or synthetic underwear traps moisture, increasing the risk of infections.
7. Stress and Sleep Deprivation
Stress weakens the immune system and increases cortisol, a hormone that promotes blood sugar spikes, thereby further fueling Candida.
8. Pesticides and Environmental Toxins
Chemical exposure from food, water, and air pollution can alter the vaginal microbiome and impair immune function.
Chapter 4: Symptoms of Vaginal Candida Overgrowth
Common symptoms include:
-
Intense vaginal itching and burning
-
Thick, white, odorless discharge (often described as “cottage cheese-like”)
-
Redness, swelling, and soreness of the vulva
-
Pain during intercourse (dyspareunia)
-
Painful urination (dysuria)
-
Recurrent infections, often monthly
Warning: These symptoms can overlap with other vaginal infections (like bacterial vaginosis or STIs). Always consult a healthcare provider for an accurate diagnosis.
Less Common But Concerning Signs:
In immunocompromised individuals, Candida can enter the bloodstream (candidemia), leading to systemic infection and even organ failure.
Chapter 5: Conventional Treatments (And Their Limits)
1. Topical Antifungals
-
Clotrimazole
-
Miconazole
-
Terconazole
These are applied inside the vagina as creams or suppositories and usually relieve symptoms within days.
2. Oral Antifungals
-
Fluconazole (Diflucan): A single-dose oral tablet often prescribed for yeast infections.
But here’s the problem:
-
Antifungals kill the yeast, but they don’t restore the microbiome.
-
This creates a cycle of temporary relief followed by recurrent infections.
-
Candida biofilms (protective layers) make them resistant to antifungal drugs over time.
-
Overuse may lead to fungal resistance and even damage liver enzymes.
3. Steroid Creams (Wrongly Prescribed)
Some women are mistakenly given corticosteroid creams, which suppress the immune response and worsen fungal growth.
4. Drawbacks of Repeated Use
-
Masking the root issue
-
Contributing to antifungal-resistant Candida strains
-
Not supporting beneficial flora recovery
Chapter 6: Probiotics as a Natural and Effective Solution
Why Probiotics?
Probiotics are live beneficial bacteria that can restore vaginal and gut microbiota. When taken orally or vaginally, they compete with Candida, acidify the environment, and reinforce the immune system.
Scientific Evidence:
A 2020 meta-analysis in Journal of Fungi found that probiotics, especially Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14, significantly reduced recurrence rates of vaginal candidiasis.
Another study in Frontiers in Microbiology showed that multi-strain probiotics helped clear infections faster when used alongside antifungal medication.
How They Work:
-
Lower vaginal pH to <4.5 (acidic, yeast-unfriendly)
-
Secreted hydrogen peroxide and bacteriocins (natural antimicrobials)
-
Restore mucosal immunity
-
Inhibit Candida adhesion to epithelial cells
-
Compete for nutrients and space
Chapter 7: The Gut-Vagina Axis
Modern science emphasizes the gut-vagina connection. Disruptions in gut flora—especially from antibiotics, poor diet, or stress—can trigger vaginal dysbiosis.
Akkermansia & Clostridium Butyricum: Advanced Allies
Akkermansia muciniphila, a mucin-loving gut bacterium, helps:
-
Restore gut lining integrity (leaky gut can exacerbate Candida)
-
Regulate immune tolerance
-
Reduce systemic inflammation, which is linked to recurrent yeast infections
Clostridium butyricum produces butyrate, a short-chain fatty acid that:
-
Inhibits fungal overgrowth
-
Reduces gut pH
-
Boosts colonization of Lactobacilli and Bifidobacteria
Together, they form a powerful support for long-term microbiome restoration.
Chapter 8: Candida Diet – What You Eat Can Heal or Harm
Foods to Avoid
-
Sugar (white sugar, honey, syrups)
-
Alcohol
-
Refined carbs (white bread, pasta, pastries)
-
Processed foods
-
Fruit juices and sweetened yogurts
Foods That Heal
-
Non-starchy vegetables
-
Garlic, coconut oil (antifungal properties)
-
Fermented foods (sauerkraut, kimchi, kefir)
-
Prebiotic-rich foods (asparagus, Jerusalem artichokes, flaxseeds)
-
High-fiber foods to feed beneficial bacteria
Diet change alone won’t cure Candida, but without dietary change, other treatments will fail.
Chapter 9: Prevention and Long-Term Healing
1. Regular Probiotic Use
Especially for women prone to recurring infections, a daily probiotic supplement with targeted vaginal strains is essential.
2. Vaginal Probiotic Suppositories
Several products now offer vaginal delivery of Lactobacillus crispatus and L. gasseri for fast and localized restoration.
3. Avoid Harsh Soaps and Douching
Stick to water or pH-balanced, unscented intimate washes.
4. Wear Breathable Cotton Underwear
Avoid sitting in wet swimwear or tight leggings for prolonged periods.
5. Manage Blood Sugar
If you have insulin resistance or PCOS, managing blood glucose will also reduce yeast-prone environments.
Chapter 10: A Holistic Approach – Microbiome-Centered Healing
Candida is not just a vaginal issue—it's a sign of a deeper microbiome imbalance and possibly immune dysregulation. Antibiotics, a poor diet, hormonal imbalances, and stress all contribute to the growth of the fungus.
The solution isn’t just "killing Candida"—it’s restoring microbial harmony.
Long-term health comes from building a robust, diverse microbiome in the gut and vagina, with the help of:
Probiotic supplements
Polyphenol-rich prebiotics
Natural antifungal foods
Gut lining repair nutrients (zinc, glutamine, omega-3s)
Probiotic-Based Solution Recommendation
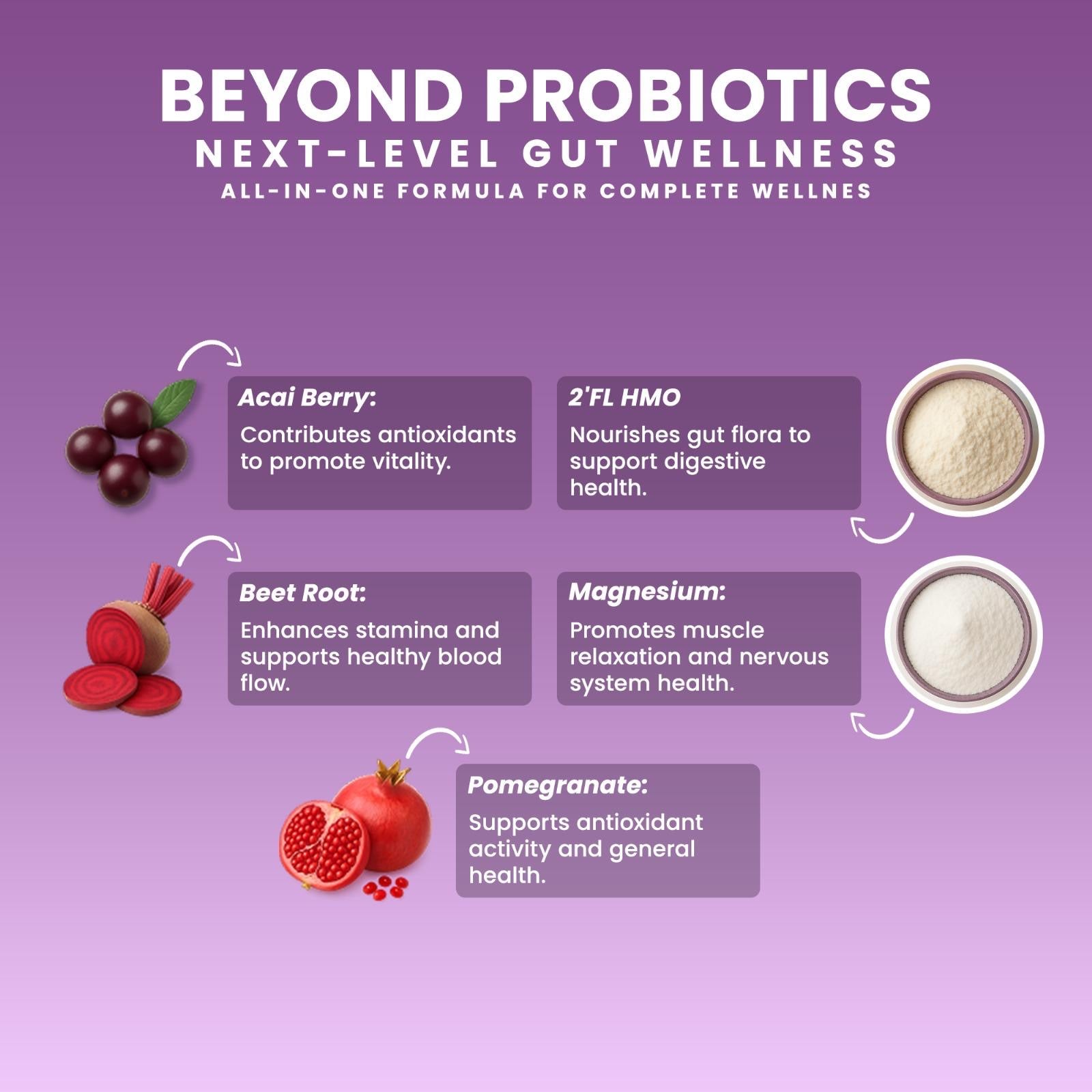
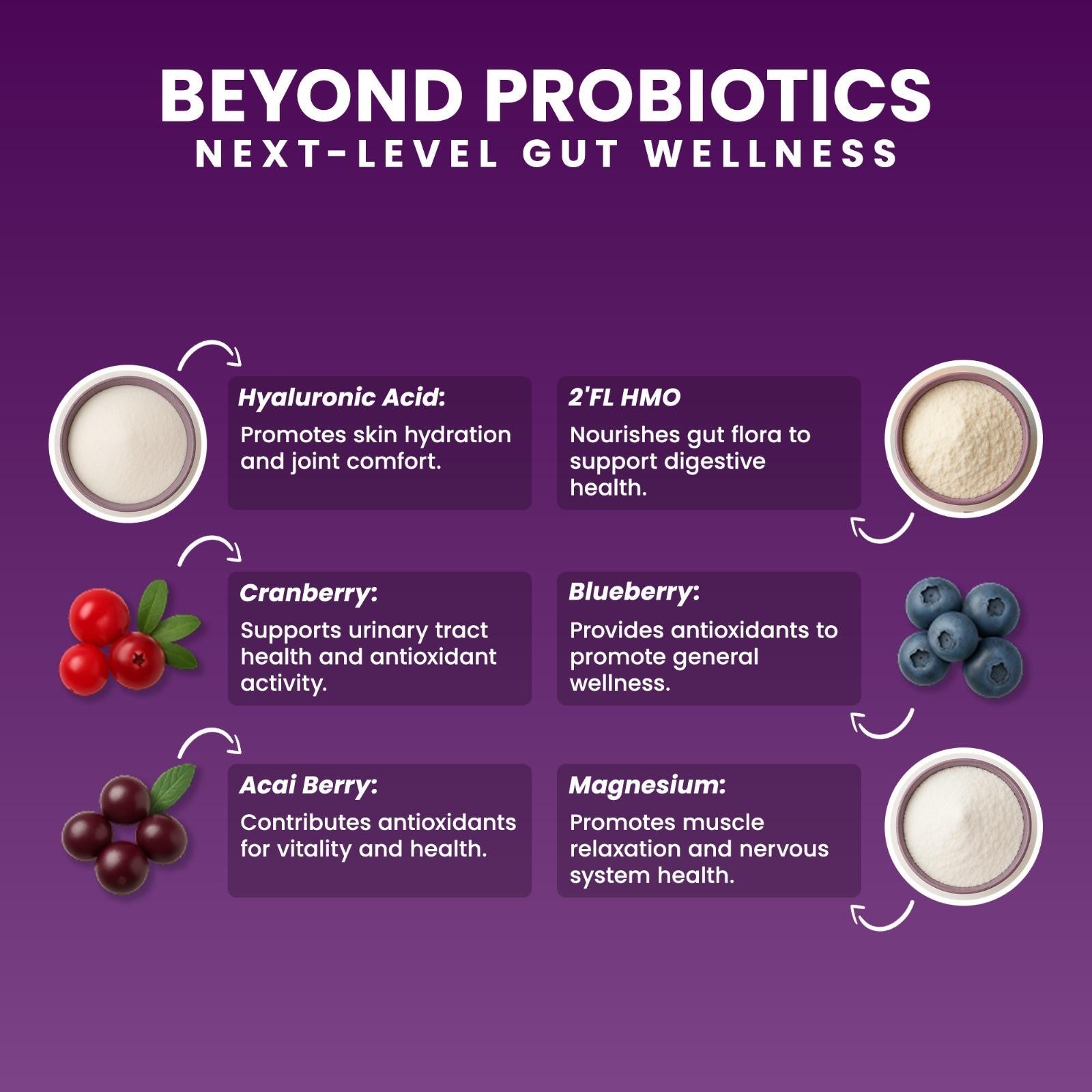
If you’re looking for a powerful yet gentle supplement, consider a formulation like Next Microbiome Akkermansia Chewable or Boost Synergy GLP-1, which includes:
-
Akkermansia muciniphila (gut lining support)
-
Clostridium butyricum (butyrate production)
-
Lactobacillus strains (vaginal flora restoration)
-
Prebiotics to feed beneficial bacteria
-
Polyphenols and plant-based antifungal extracts
🔗 Akkermansia Chewable (Probiome Novo 2.0)
🔗 Boost Synergy GLP-1 Probiotic
Conclusion: From Disruption to Balance
Vaginal Candida infections are not just minor nuisances. They are signals—urgent messages from your microbiome that something is off. The good news? Nature has solutions.
With the right diet, hygiene habits, lifestyle changes, and probiotic supplementation, it’s possible to break the cycle of recurrent infections and rebuild a resilient ecosystem—one that supports long-term vaginal and whole-body health.
Final Tip:
Always consult your healthcare provider before starting any new treatment, especially if you’re pregnant, immunocompromised, or on other medications.