Microbiome Development: How Early Life Shapes Health
Microbiome Development From Birth to Adulthood: How Early Life Shapes Lifetime Health
The human microbiome is not something we’re simply born with — it develops over time through a series of critical stages. From birth to age three, the microbiome undergoes rapid, influential changes that shape immunity, digestion, metabolic resilience, and even lifelong disease risk.
As we move through childhood, adulthood, and aging, the microbiome continues to evolve in response to diet, environment, stress, medication, and lifestyle.
If you haven’t explored the foundational articles in this cluster, start here:
👉 What Is the Human Microbiome? A Complete Guide to Microbes, Immunity & Digestion
👉 Oral Microbiota & Gut Health: How the Mouth Shapes the Entire Microbiome
👉 The Gut–Brain Axis: How Microbes Influence Mood, Stress & Appetite
Now let’s explore how your microbiome develops — and why early life is the most critical window of all.
Common Questions
1. When does the microbiome begin developing?
At birth, within seconds of delivery.
2. Can early-life microbiome disruption affect adulthood?
Yes, research shows early dysbiosis influences allergies, immunity, metabolism, and inflammation later in life.
3. Do oral microbes affect early microbiome development?
Absolutely — infants’ oral bacteria directly seed the gut microbiome.
4. What foods support microbiome development?
Polyphenols, fiber-rich foods, fermented foods, and prebiotics.
5. What weakens childhood or adult microbiomes?
Antibiotics, ultra-processed foods, stress, poor sleep, low fiber, and environmental toxins.
6. Can the microbiome still be improved in adulthood?
Yes — the microbiome is highly adaptable and responds quickly to diet and supplements.
The Microbiome at Birth: The First Colonization Event
The moment we are born, our bodies begin acquiring microbes.
A landmark open-access review describes how infant microbiota development shapes lifelong immunity:
📚 The Role of Microbiota in Infant Health — Yao et al., 2021
👉 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8529064/
Key determinants at birth include:
✔ Mode of delivery
-
Vaginal birth: Highest microbial diversity; exposure to maternal microbes
-
C-section: Delayed colonization; greater risk of dysbiosis
✔ Early feeding
-
Breastfeeding: Rich in HMOs (especially 2'-FL) → feeds beneficial microbes
-
Formula: Different microbial pathways; often less diversity
✔ Environment
-
Skin-to-skin contact
-
Household microbial exposure
-
Pets, siblings, surfaces
Birth is the first major seeding of microbial identity.

The Microbiome in Early Childhood: Ages 0–3
This period is the most critical window for microbiome programming.
During this time:
-
Microbial diversity expands
-
Immune tolerance develops
-
Oral–gut axis becomes established
-
The gut lining matures
-
Mucin production stabilizes
-
SCFA pathways activate
Infants exposed to diverse microbes develop stronger immune systems and lower inflammation later in life.
Disruptions — such as antibiotics, stress, lack of polyphenols, or poor diet — may lead to:
-
allergies
-
eczema
-
asthma
-
food sensitivities
-
digestive issues
-
metabolic problems later on
The Oral–Gut Axis in Infancy
The mouth is the gateway to the infant microbiome.
Oral bacteria strongly shape early microbial colonization because infants:
-
explore objects orally
-
transfer microbes to the gut through saliva
-
receive microbial exposures through breastfeeding
-
share oral microbes with caregivers
📚 Oral–Gut Microbiome Interaction — Frontiers (2021)
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC8125773/
Supporting oral microbial health early on helps stabilize gut colonization patterns.
The Microbiome in Childhood
Childhood dietary and environmental exposures determine microbial “training.”
Key influences:
-
fiber intake
-
exposure to natural environments
-
early socialization
-
sleep
-
stress levels
-
antibiotic usage
-
family diet
Children with high microbial diversity generally have:
-
stronger immunity
-
lower inflammation
-
better digestion
-
healthier metabolic patterns
The childhood microbiome sets the stage for lifelong resilience.

The Microbiome in Adolescence & Early Adulthood
During adolescence:
-
Hormonal shifts change microbial composition
-
Stress begins to influence gut–brain pathways
-
Food choices shape inflammation
-
Oral microbiota becomes more stable
-
Gut lining integrity strengthens — or becomes compromised
By adulthood, the microbiome becomes relatively stable, though still modifiable.
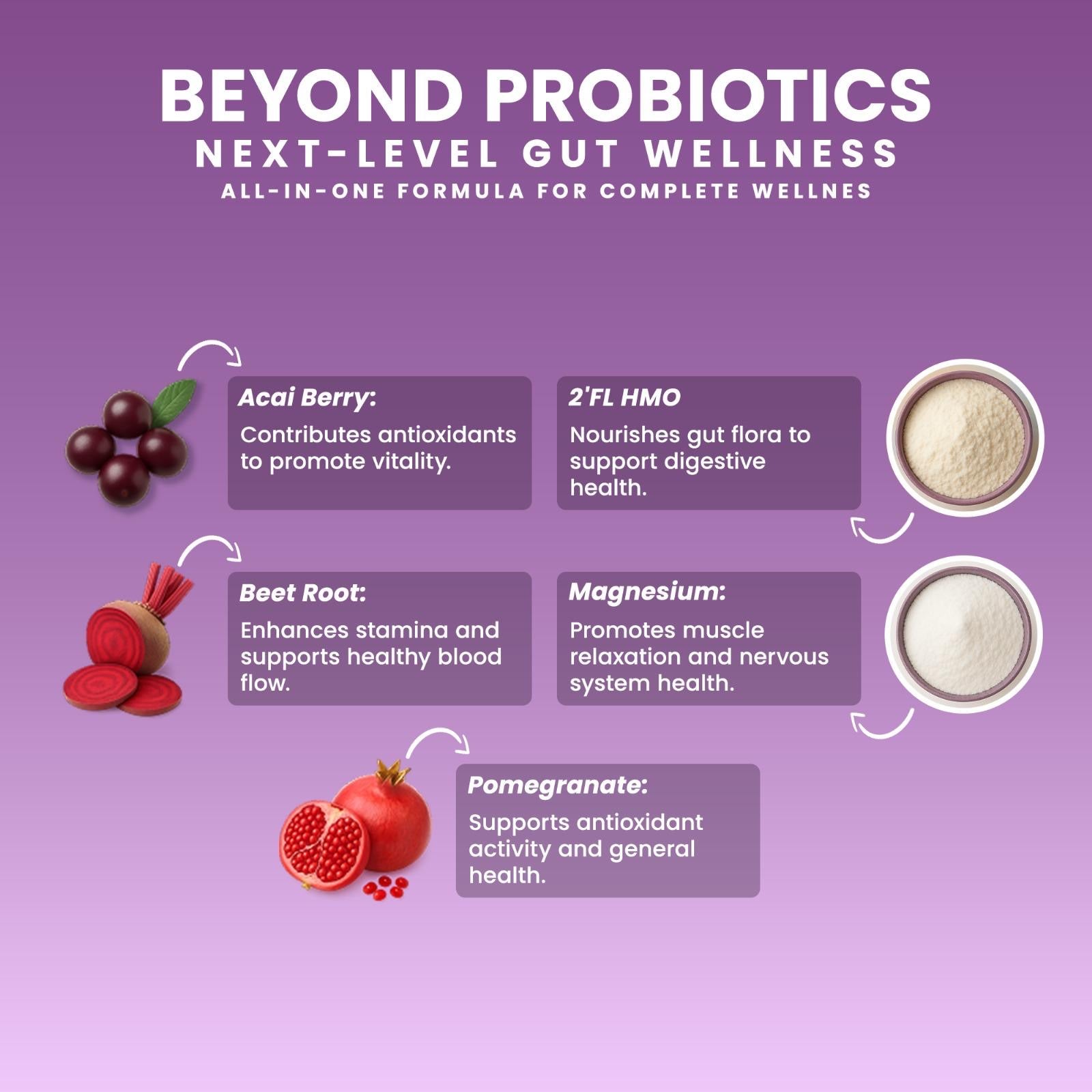
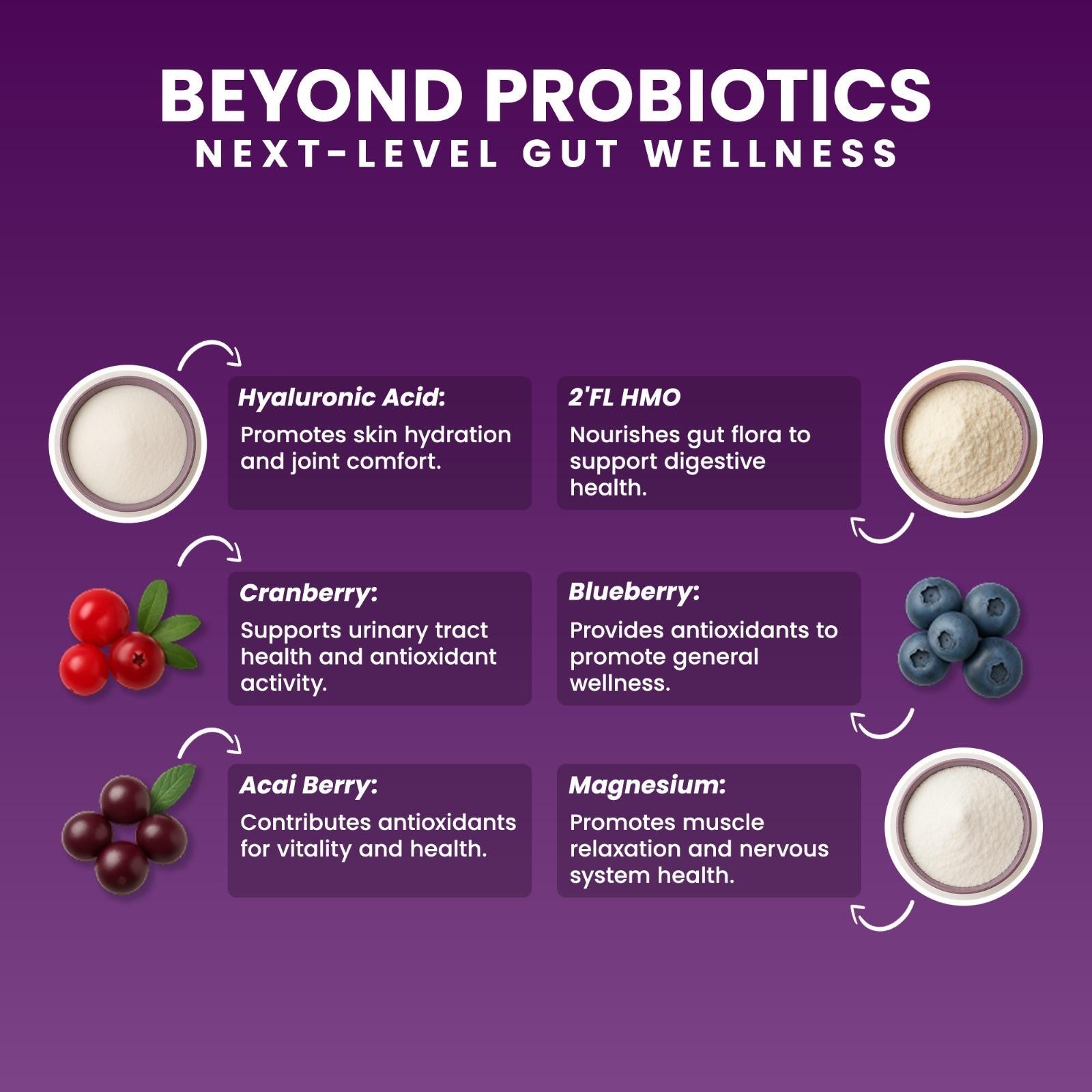
Factors that strengthen the adult microbiome:
-
high-fiber, plant-rich diets
-
polyphenols (berries, cocoa, pomegranate)
-
SCFA-supportive probiotics
-
HMOs (2’-FL) for mucosal health
-
sleep & stress balance
-
supporting the oral–gut axis (chewable formats)
📚 Polyphenols & Microbiota — Wang et al., 2022
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC9220293/
The Microbiome in Aging
As we age:
-
Microbial diversity declines
-
SCFA production decreases
-
Inflammation increases
-
Gut-lining integrity weakens
-
Immune function declines
-
Oral dysbiosis becomes more common
Supporting the microbiome becomes essential for:
-
metabolic health
-
brain health
-
immune protection
-
inflammation reduction
Older adults benefit significantly from:
-
probiotics
-
prebiotics
-
polyphenols
-
lifestyle improvements
-
oral microbiota support
How to Support Microbiome Health Across All Ages
✔ Polyphenols
(Foods that support microbial diversity & mucin health)
https://pmc.ncbi.nlm.nih.gov/articles/PMC9220293/
✔ Prebiotics
(Inulin, FOS, resistant starch — feed beneficial bacteria)
✔ HMOs (2’-FL)
(Strengthen infant & adult mucosal immunity)
https://pmc.ncbi.nlm.nih.gov/articles/PMC6164445/
✔ SCFA-supportive probiotics
(Clostridium butyricum)
Increase butyrate to support epithelial repair.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8078720/
✔ Oral–gut microbiota support
(Chewables activate the microbiome early in the digestive process)
✍️ Written by Ali Rıza Akın
Microbiome Scientist, Author & Founder of Next-Microbiome
Ali Rıza Akın is a microbiome scientist with nearly 30 years of Silicon Valley biotechnology and translational research experience. He is the discoverer of Christensenella californii, a novel human-associated microbial species linked to mucosal and metabolic health.
His scientific expertise includes:
• mucosal immunology
• gut barrier biology
• oral–gut microbiome interactions
• SCFA metabolism
• next-generation probiotics (Akkermansia, Christensenella, Clostridium butyricum)
• host–microbe signaling
• translational microbial therapeutics
He authored Bakterin Kadar Yaşa: İçimizdeki Evren and contributed to Bacterial Therapy of Cancer: Methods and Protocols (Springer).
As Founder of Next-Microbiome, he develops advanced synbiotic formulations — including the first chewable Akkermansia-supporting synbiotic — engineered to strengthen the gut lining, support metabolic resilience, and harmonize the oral–gut axis.