The Gut–Brain Axis: How Microbes Shape Mood & Appetite
The Gut–Brain Axis: How Microbes Influence Mood, Stress & Appetite
For decades, scientists believed the brain controlled the gut.
Today, we know the truth:
The gut speaks to the brain just as much — and sometimes even louder.
This connection is called the gut–brain axis, a two-way communication network powered by:
-
gut microbes
-
vagus nerve signaling
-
immune pathways
-
microbial neurotransmitters
-
hormonal regulation
-
inflammatory molecules
Your gut doesn’t just digest food — it influences how you think, feel, sleep, and respond to stress.
If you haven’t read the foundation of microbiome science yet, start with:
👉 What Is the Human Microbiome? A Complete Guide to Microbes, Immunity & Digestion
And if you'd like to understand how digestion truly begins in the mouth, continue with:
👉 Oral Microbiota & Gut Health: How the Mouth Shapes the Entire Microbiome
Now let’s explore how your gut microbes shape your emotional world.
Common Questions
1. Can gut bacteria really affect my mood?
Yes — through neurotransmitters, inflammation control, vagus signaling, and hormonal pathways.
2. Can stress change my microbiome?
Absolutely. Stress hormones weaken the integrity of the gut lining and alter microbial composition.
3. Does improving gut health improve anxiety?
Many people experience reduced anxiety when improving gut microbial balance.
4. Is the oral microbiome connected to the gut–brain axis?
Yes — oral bacteria influence gut inflammation, which influences brain signaling.
5. Which foods support the gut–brain axis?
Polyphenols, fiber, fermented foods, omega-3 sources, and green tea.
6. Do chewable probiotics help the gut–brain axis?
Yes — because they activate in the mouth, improving oral–gut–brain communication.
What Is the Gut–Brain Axis?
The gut–brain axis (GBA) is the constant communication loop between the digestive system and the central nervous system.
This network includes:
-
the vagus nerve
-
gut microbes
-
immune cells
-
neurotransmitters
-
hormones
-
epithelial cells
-
brain centers for emotion & memory
📚 Scientific Reference:
Microbiota–Gut–Brain Axis — Physiological Reviews (2018)
👉 https://journals.physiology.org/doi/abs/10.1152/physrev.00018.2018
This paper confirms that microbes influence mood, appetite, stress response, and cognitive performance.

How Gut Microbes Talk to the Brain
Microbes communicate with the brain through several biological channels:
1. Neurotransmitter Production
The gut produces:
-
90% of the body's serotonin
-
50% of the body’s dopamine
-
GABA
-
Acetylcholine
These regulate:
-
mood
-
motivation
-
reward
-
stress resilience
-
sleep
-
digestion
2. Vagus Nerve Signaling
The vagus nerve is the “information highway” between gut and brain.
Healthy microbes → calming signals
Dysbiosis → stress signals
This is why gut discomfort often worsens anxiety — and why anxiety worsens digestion.
3. Immune Pathways
Inflammation is a major driver of mood disorders.
The microbiome regulates inflammation by:
-
training immune cells
-
maintaining gut lining integrity
-
reducing toxic metabolites
-
preventing cytokine overactivity
A healthier microbiome = a calmer immune system = a calmer brain.
4. Microbial Metabolites (SCFAs)
Short-chain fatty acids (SCFAs), especially butyrate, influence:
-
neuroinflammation
-
brain-derived neurotrophic factor (BDNF)
-
learning
-
stress recovery
-
resilience to depression
📚 SCFA Reference:
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC8078720/
5. Hormonal Regulation
Microbes regulate:
-
cortisol
-
ghrelin
-
leptin
-
GLP-1
This influences:
-
appetite
-
energy
-
cravings
-
stress
-
emotional stability
How Dysbiosis (Microbiome Imbalance) Affects the Brain
When the microbiome becomes imbalanced, people often experience:
-
anxiety
-
stress reactivity
-
low mood
-
irritability
-
cravings
-
sleep disturbances
-
poor focus
-
digestive flare-ups
This is not psychological —
it is biological.
Dysbiosis → inflammation → disrupted gut lining → altered neurotransmitters → vagus nerve stress → brain imbalance.
The Oral–Gut–Brain Connection
The gut–brain axis does NOT start in the gut.
It starts in the mouth.
Oral bacteria influence:
-
vagus nerve tone
-
nitric oxide pathways
-
immune activation
-
upper-GI microbial balance
📚 Reference:
Oral–Gut Microbiome Interaction
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC8125773/
This means:
Healthy oral microbiota → healthier gut → healthier brain
Oral dysbiosis → inflamed gut → stressed brain
This is why chewable microbiome supplements engage the gut–brain axis more effectively than capsules.
Foods That Support the Gut–Brain Axis
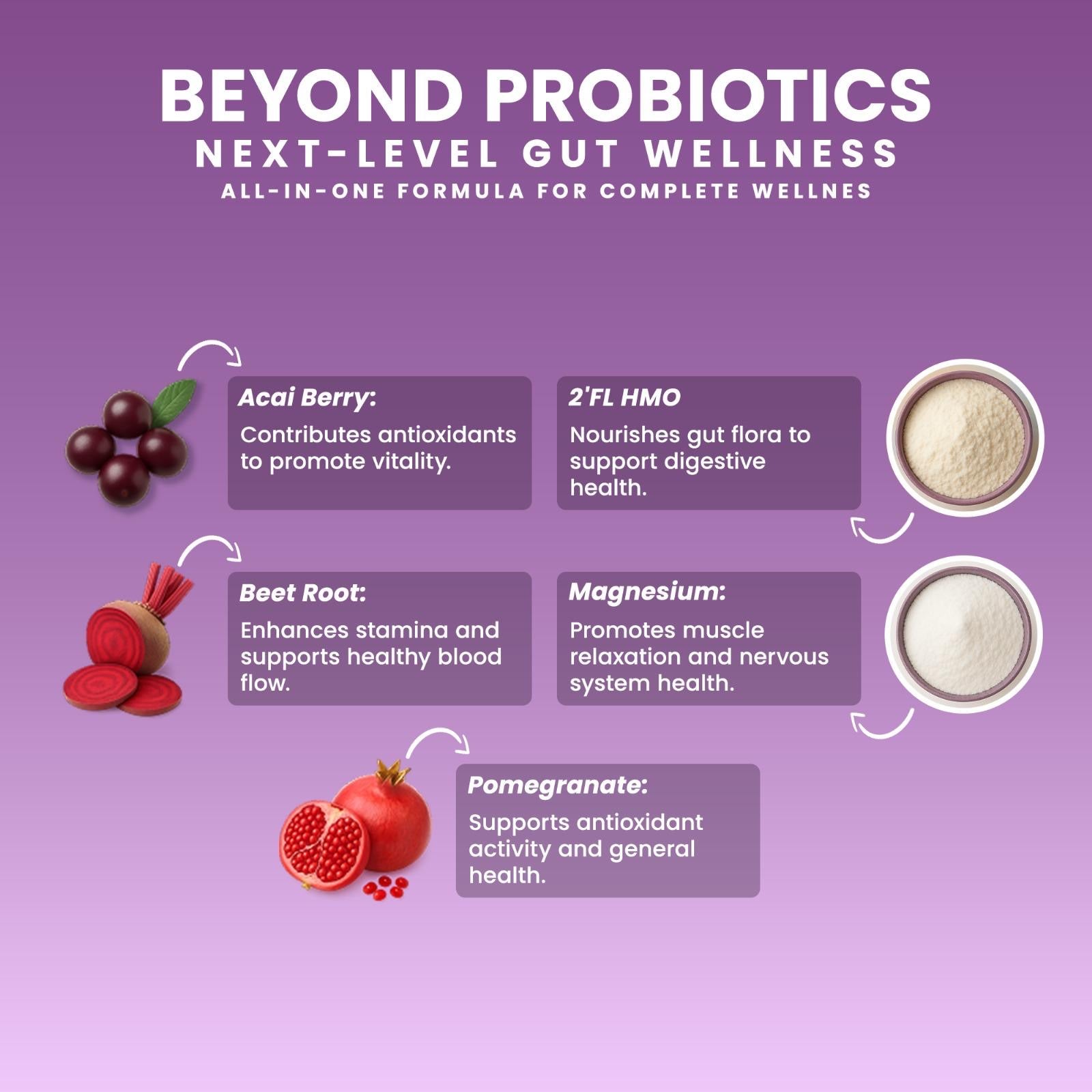
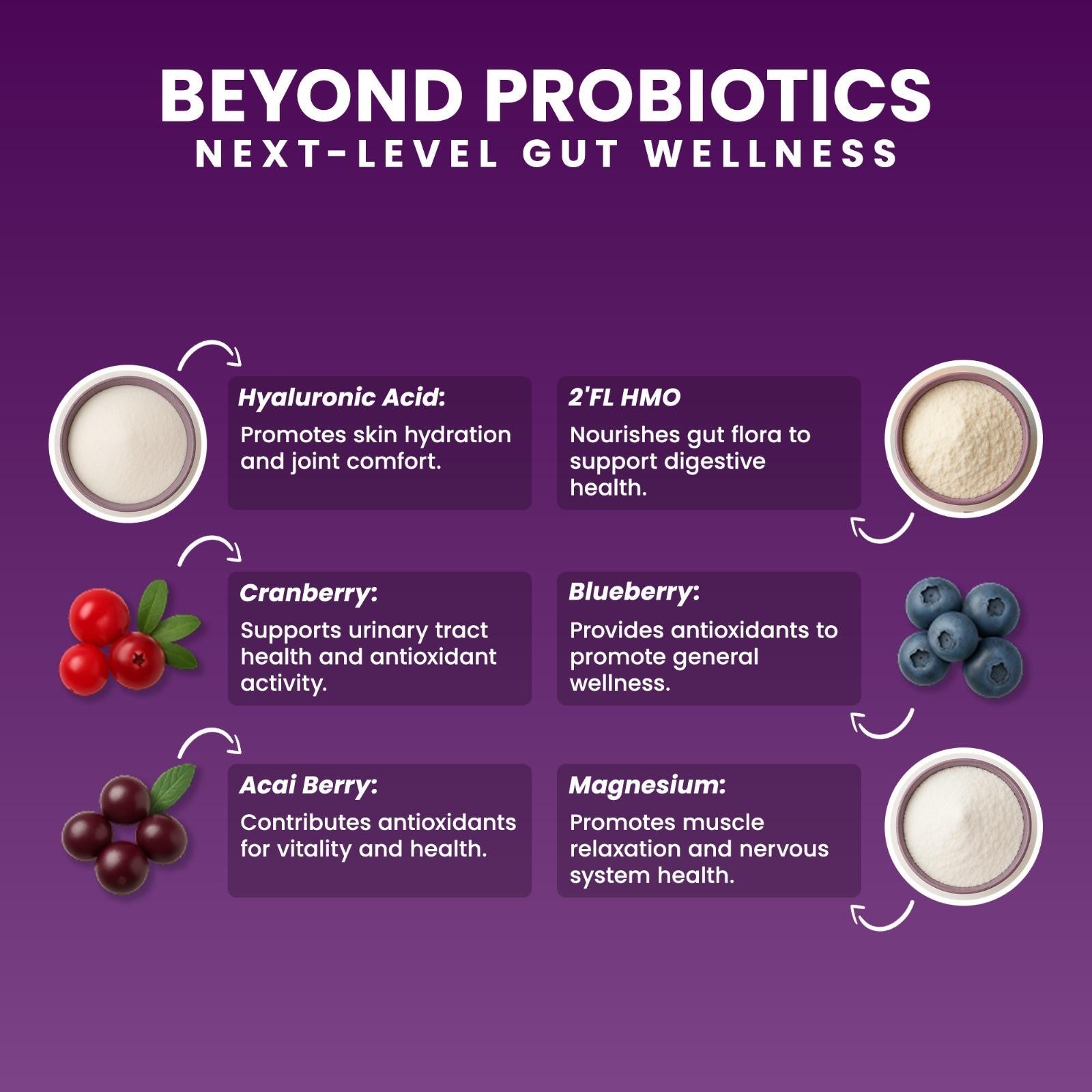
1. Polyphenols
Found in berries, cocoa, pomegranate, green tea.
They increase beneficial microbes, reduce inflammation, and support cognition.
📚 Reference:
Dietary Polyphenol & Gut Microbiota — Wang et al.
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC9220293/
2. Prebiotics
Such as inulin, FOS, resistant starch.
They feed beneficial bacteria & increase SCFAs.
3. Human Milk Oligosaccharides (HMOs)
Especially 2’-FL, supporting mucosal immunity & microbial signaling.
📚 HMO Reference:
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC6164445/
4. SCFA-Supportive Probiotics
Including Clostridium butyricum, which enhances butyrate production.
📚 SCFA Reference:
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC8078720/
5. Chewable Microbiome Formulas
They influence the oral microbiota first → then the gut → then the brain.
✍️ Written by Ali Rıza Akın
Microbiome Scientist, Author & Founder of Next-Microbiome
Ali Rıza Akın is a microbiome scientist with nearly 30 years of biotechnology and translational research experience in Silicon Valley. He is the discoverer of Christensenella californii, a novel human-associated microbial species linked to metabolic and mucosal health.
His scientific expertise spans:
• mucosal immunology
• oral–gut microbiome interactions
• SCFA metabolism
• gut barrier biology
• next-generation probiotics (Akkermansia, Christensenella, Clostridium butyricum)
• host–microbe communication
• translational microbiome science
He is the author of Bakterin Kadar Yaşa: İçimizdeki Evren (Live as Long as Your Bacteria) and a contributor to Bacterial Therapy of Cancer: Methods and Protocols (Springer).
As the Founder of Next-Microbiome, Ali develops advanced synbiotic formulations — including the first chewable Akkermansia-supporting synbiotic — designed to strengthen the gut lining, support mucosal immunity, and optimize the oral–gut–brain axis.