Oral Microbiota & Gut Health: How the Mouth Shapes Microbiome
Oral Microbiota & Gut Health: How the Mouth Shapes the Entire Microbiome
Most people think gut health starts in the stomach or intestines —
But the truth is, digestion begins in the mouth, and the microbiome begins there, too.
Every day, more than 1 billion oral bacteria travel from the mouth down the digestive tract. These microbes influence stomach acidity, immune signals, inflammatory responses, and even the success of probiotics.
To understand the bigger picture of the human microbiome first start with:
👉 What Is the Human Microbiome? A Complete Guide to Microbes, Immunity & Digestion
Now, let’s explore why the oral microbiota is one of the most influential — and overlooked — parts of gut health.
Common Questions
1. Does the oral microbiome affect gut health?
Yes — oral bacteria migrate into the gut daily and influence acidity, immunity, inflammation, and microbial balance.
2. Can oral dysbiosis cause digestive issues?
Absolutely. Studies show it can trigger small intestinal inflammation and microbial imbalance.
3. Why is saliva important?
It transports enzymes and bacteria that initiate digestion and immune signaling.
4. Are chewable probiotics better?
Yes, because they support oral microbiota before reaching the stomach, improving downstream effects.
5. What foods support oral microbiota?
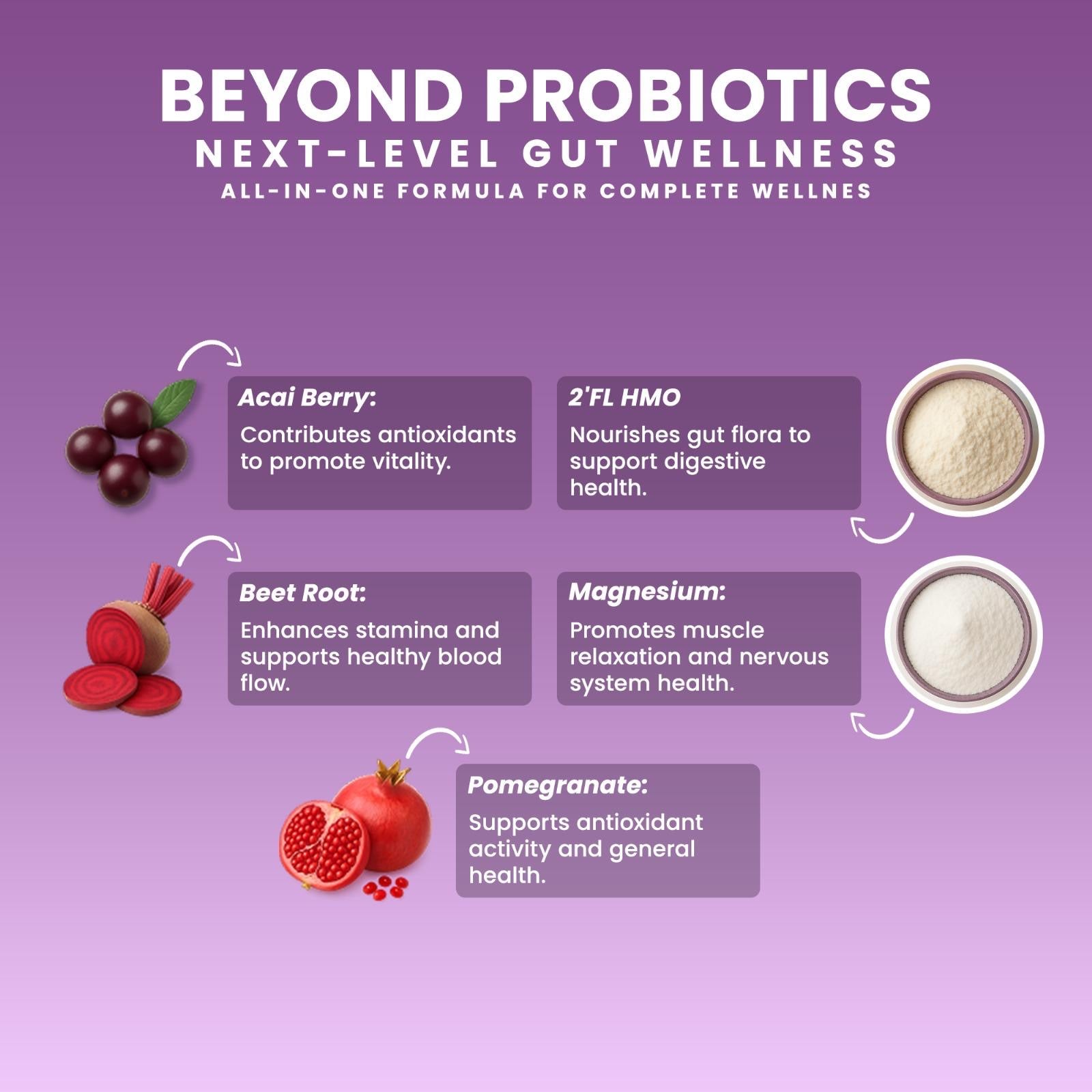
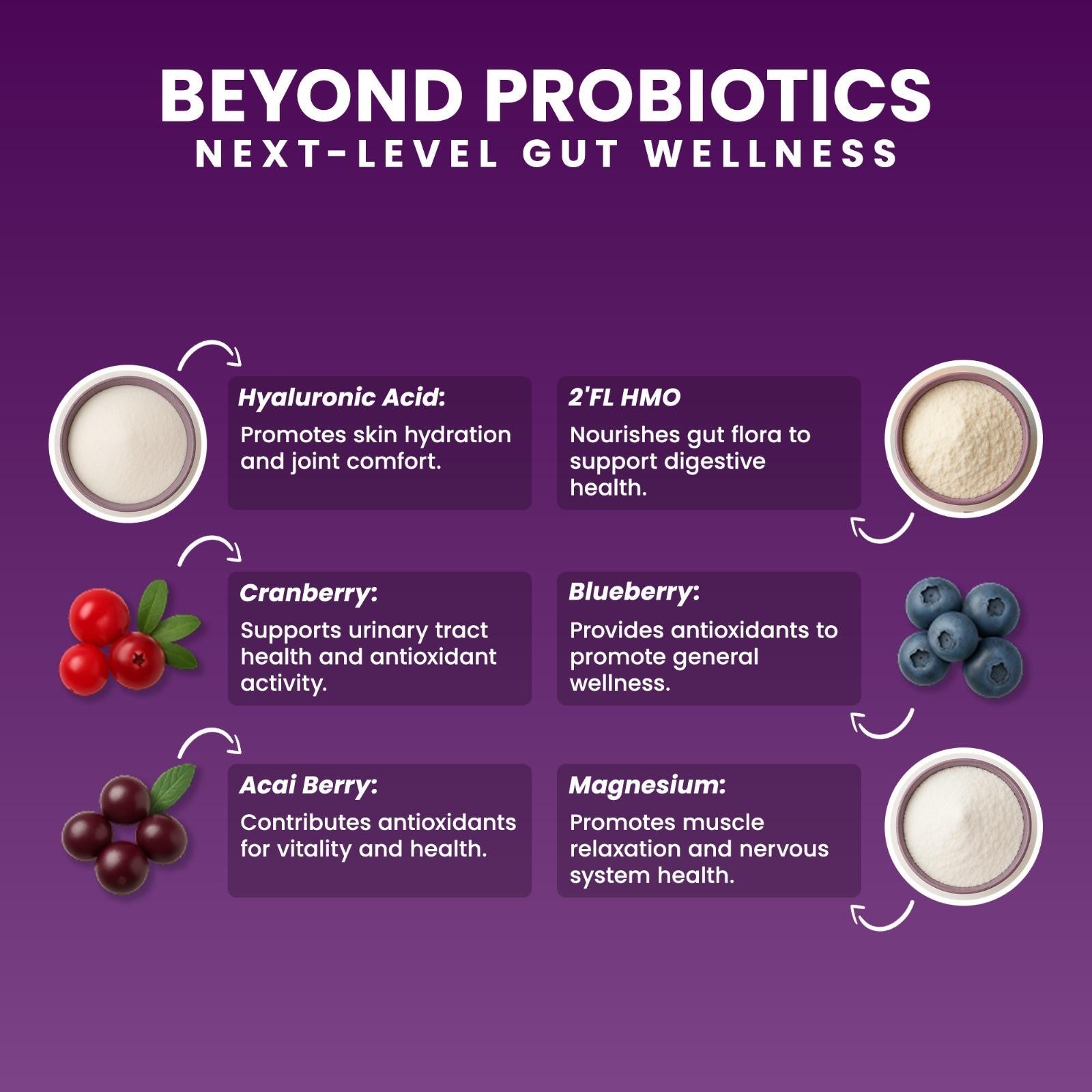
Polyphenol-rich foods: berries, cocoa, pomegranate, green tea.
6. Can improving oral microbiota improve gut health?
Yes — reducing oral inflammation and balancing oral bacteria improves gut resilience.
What Is the Oral Microbiota?
The oral microbiota consists of more than 700 microbial species living on:
-
the tongue
-
gums
-
teeth
-
tonsils
-
saliva
-
inner cheeks
This ecosystem:
-
breaks down food
-
activates digestive enzymes
-
regulates pH
-
interacts with immune cells
-
produces signaling molecules
-
primes the digestive tract
The oral cavity is a microbial “launch pad” for everything that happens downstream.
How Oral Bacteria Travel to the Gut
Scientific evidence confirms that oral bacteria routinely migrate into the gastrointestinal tract.
📚 Reference:
Oral–Gut Microbiome Interaction — Frontiers (2021)
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC8125773/
Key findings:
-
Saliva transports oral bacteria with every swallow
-
Many survive stomach acidity
-
They colonize the upper GI tract
-
They influence gut microbial diversity
-
Oral dysbiosis can cause gut dysbiosis
-
Oral pathogens increase GI inflammation
The oral microbiota is not separate from the gut — it feeds into it.

How the Oral Microbiota Shapes Gut Health
1. It Influences Stomach pH
Salivary enzymes activate before food reaches the stomach, shaping acidity and digestion speed.
2. It Primes Immune Responses
Oral bacteria interact with mucosal immune cells.
When unhealthy, they send “danger signals” downstream.
3. It Impacts Microbial Colonization
Healthy oral bacteria → healthy upper-GI colonization
Unhealthy oral bacteria → inflammatory microbial imbalance
4. It Drives Upper-GI Inflammation
Oral pathogens such as Fusobacterium and Prevotella are linked to:
-
gastritis
-
acid sensitivity
-
mucosal irritation
-
reduced microbial diversity
5. It Affects Gut Lining Strength
Oral bacteria influence mucin breakdown and tight-junction stability — affecting permeability.
The Oral–Gut Axis & the Gut–Brain Axis
The oral–gut axis directly affects the microbiota–gut–brain axis.
Changes in oral microbiota modify:
-
vagus nerve signaling
-
appetite regulation
-
stress response
-
serotonin activity
-
inflammatory signals
-
cognitive function
📚 Reference:
Microbiota–Gut–Brain Axis — Physiological Reviews (2018)
👉 https://journals.physiology.org/doi/abs/10.1152/physrev.00018.2018
This makes oral–gut health central to emotional and metabolic resilience.
Why Chewable Microbiome Formulas Work Better
Chewable microbiome supplements activate in the mouth, not just in the gut.
A chewable format can:
-
support oral microbial balance
-
activate digestive enzymes early
-
strengthen immune priming
-
reduce upper-GI inflammation
-
improve probiotic survival
-
enhance downstream gut colonization
Capsules bypass the oral microbiota entirely.
This is why formulations designed for the oral–gut axis can produce broader microbiome benefits.
How to Support the Oral Microbiota Naturally
1. Eat Polyphenol-Rich Foods
Berries, cocoa, green tea, and pomegranate support beneficial oral bacteria.
📚 Dietary Polyphenols & Gut Microbiota — Wang et al., 2022
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC9220293/
2. Reduce Oral Inflammation
Inflamed gums contribute to systemic and gut inflammation.
Improve by:
-
flossing
-
brushing gently
-
avoiding sugared drinks
-
limiting harsh alcohol-based mouthwashes
3. Strengthen the Gut Lining
When the gut lining is stable, inflammatory feedback to the mouth decreases.
HMOs (2'-FL) and SCFA-supportive probiotics help.
📚 HMO 2’-FL — AJCN
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC6164445/
📚 SCFA Support — C. butyricum
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC8078720/
4. Use a Chewable Microbiome Formula
Chewables help synchronize:
Oral Microbiota → Gut Microbiota → Gut Lining → Brain Signals
This matches natural digestion pathways.
Where This Fits in the Human Microbiome Cluster
If you’re exploring the microbiome step-by-step, continue your learning journey:
👉 What Is the Human Microbiome? A Complete Guide to Microbes, Immunity & Digestion
👉 Oral Microbiota & Gut Health: How the Mouth Shapes the Entire Microbiome
👉 The Gut–Brain Axis: How Microbes Influence Mood, Stress & Appetite
👉 Microbiome Development From Birth to Adulthood
✍️ Written by Ali Rıza Akın
Microbiome Scientist, Author & Founder of Next-Microbiome
Ali Rıza Akın is a microbiome scientist with nearly 30 years of biotechnology and translational research experience in Silicon Valley. He is the discoverer of Christensenella californii, a novel human-associated microbial species linked to metabolic and mucosal health.
His scientific expertise spans:
• mucosal immunology
• oral–gut microbiome interactions
• SCFA metabolism
• gut barrier biology
• next-generation probiotics (Akkermansia, Christensenella, Clostridium butyricum)
• host–microbe communication
• microbial therapeutics & translational microbiome science
Ali is the author of Bakterin Kadar Yaşa: İçimizdeki Evren (Live as Long as Your Bacteria) and a contributor to Bacterial Therapy of Cancer: Methods and Protocols (Springer).
As the Founder of Next-Microbiome, he develops advanced synbiotic formulations — including the first chewable Akkermansia-supporting synbiotic — designed to strengthen the gut lining, enhance mucosal immunity, support the oral–gut axis, and improve metabolic resilience.