What Is the Human Microbiome? Microbes, Immunity & Digestion
What Is the Human Microbiome? A Complete Guide to Microbes, Immunity & Digestion
The human microbiome is a vast, dynamic ecosystem of trillions of microorganisms — including bacteria, fungi, archaea, and viruses — that live throughout the body, especially in the gut. These microbes play essential roles in digestion, immunity, inflammation, metabolism, oral health, and even mood and cognitive performance.
Modern research shows the microbiome behaves like an additional organ system, continuously communicating with intestinal cells, immune receptors, metabolic hormones, and the nervous system.
Understanding the microbiome is foundational to understanding your overall health.
Common Questions
1. What is the human microbiome?
A dynamic ecosystem of microorganisms living throughout the body that influence digestion, immunity, metabolism, inflammation, and even brain health.
2. How does the microbiome support digestion?
By breaking down fibers, resistant starches, and polyphenols into short-chain fatty acids that strengthen the gut lining and support nutrient absorption.
3. What weakens the microbiome?
Antibiotics, chronic stress, poor sleep, processed foods, alcohol, low fiber, toxins, and artificial sweeteners.
4. How does the microbiome influence the brain?
Through the gut–brain axis, involving the vagus nerve, microbial neurotransmitters, immune signals, and microbial metabolites.
5. How can I improve my microbiome naturally?
Increase fiber and polyphenols, use prebiotics and SCFA-supportive probiotics, support HMOs like 2’-FL, reduce stress, sleep well, and minimize ultra-processed foods.
6. Why is oral microbiota important for gut health?
Oral bacteria migrate to the gut daily and shape digestive enzymes, inflammatory patterns, microbial colonization, and immune responses.
The Human Microbiome: A Map of Invisible Life
The landmark Human Microbiome Project (HMP), published in Nature, created the most comprehensive map of microbial communities across the human body:
👉 Structure, function and diversity of the healthy human microbiome — Nature
https://www.nature.com/articles/nature11234
Key insights from HMP include:
-
Every person has a unique microbial “fingerprint.”
-
Higher microbial diversity is linked to healthier immune and metabolic profiles.
-
Dysbiosis (microbial imbalance) contributes to inflammation, digestive disorders, and metabolic dysfunction.
-
Distinct body regions host specialized microbial communities (gut, mouth, skin, lungs, reproductive tract).
Your microbiome evolves constantly in response to diet, lifestyle, stress, medication, and environment.

What the Microbiome Does for Your Health
1. Drives Digestion & Nutrient Breakdown
Microbes break down fibers, resistant starches, and polyphenols into beneficial metabolites.
📚 BMJ — The gut microbiome in health & disease
https://www.bmj.com/content/361/bmj.k2179
2. Regulates the Immune System
About 70% of the immune system resides in the gut lining. Microbes help train immune responses and reduce unnecessary inflammation.
3. Protects the Gut Lining
Microbial communities maintain:
-
the mucin barrier
-
epithelial cell renewal
-
tight-junction stability
A healthy microbiome = a stronger intestinal barrier.
4. Produces SCFAs (Short-Chain Fatty Acids)
SCFAs such as butyrate:
-
fuel colon cells
-
repair the mucosal barrier
-
regulate immune balance
-
improve metabolic function
5. Supports Metabolic Health
Microbes regulate:
-
appetite hormones
-
glucose response
-
fat storage
-
inflammation
-
metabolic flexibility
6. Communicates With the Brain (The Gut–Brain Axis)
Microbes influence mood, stress, and cognition through:
-
the vagus nerve
-
neurotransmitters
-
immune signaling
-
microbial metabolites
📚 Microbiota–Gut–Brain Axis — Physiological Reviews (2018)
https://journals.physiology.org/doi/abs/10.1152/physrev.00018.2018
The Gut Microbiome: Your Most Powerful Microbial Organ
The gut hosts the densest microbial population in the human body.
It influences:
-
digestion
-
nutrient absorption
-
inflammation control
-
hormone production
-
mucosal immunity
-
metabolic regulation
A diverse gut microbiome is strongly associated with better overall health.
The Oral–Gut Microbiome Axis: Digestion Starts Before the Stomach
Digestion begins in the mouth, not the stomach.
More than 1 billion oral bacteria enter the gut daily and shape:
-
stomach acidity
-
upper-GI inflammation
-
microbial colonization
-
enzyme activation
-
immune priming
📚 Oral–Gut Microbiome Interaction — Frontiers (2021)
https://pmc.ncbi.nlm.nih.gov/articles/PMC8125773/
This is why chewable microbiome formulas can activate digestive and immune pathways earlier than capsules.
Microbiome Development: From Birth to Adulthood
Early-life microbial colonization sets the foundation for long-term immune, digestive, and metabolic health.
📚 The Role of Microbiota in Infant Health — Yao et al., 2021
https://pmc.ncbi.nlm.nih.gov/articles/PMC8529064/
Influencing factors include:
-
birth mode (vaginal vs. C-section)
-
breastfeeding vs. formula
-
early antibiotics
-
introduction of solid foods
-
home environment
-
infections
These shape immunity, inflammation, and metabolic resilience into adulthood.
What Damages the Microbiome?
Common disruptors include:
-
antibiotics
-
chronic stress
-
ultra-processed foods
-
alcohol
-
low fiber intake
-
artificial sweeteners
-
poor sleep
-
environmental toxins
-
chronic inflammation
These reduce microbial diversity and weaken the gut lining.

How to Support a Healthy Microbiome
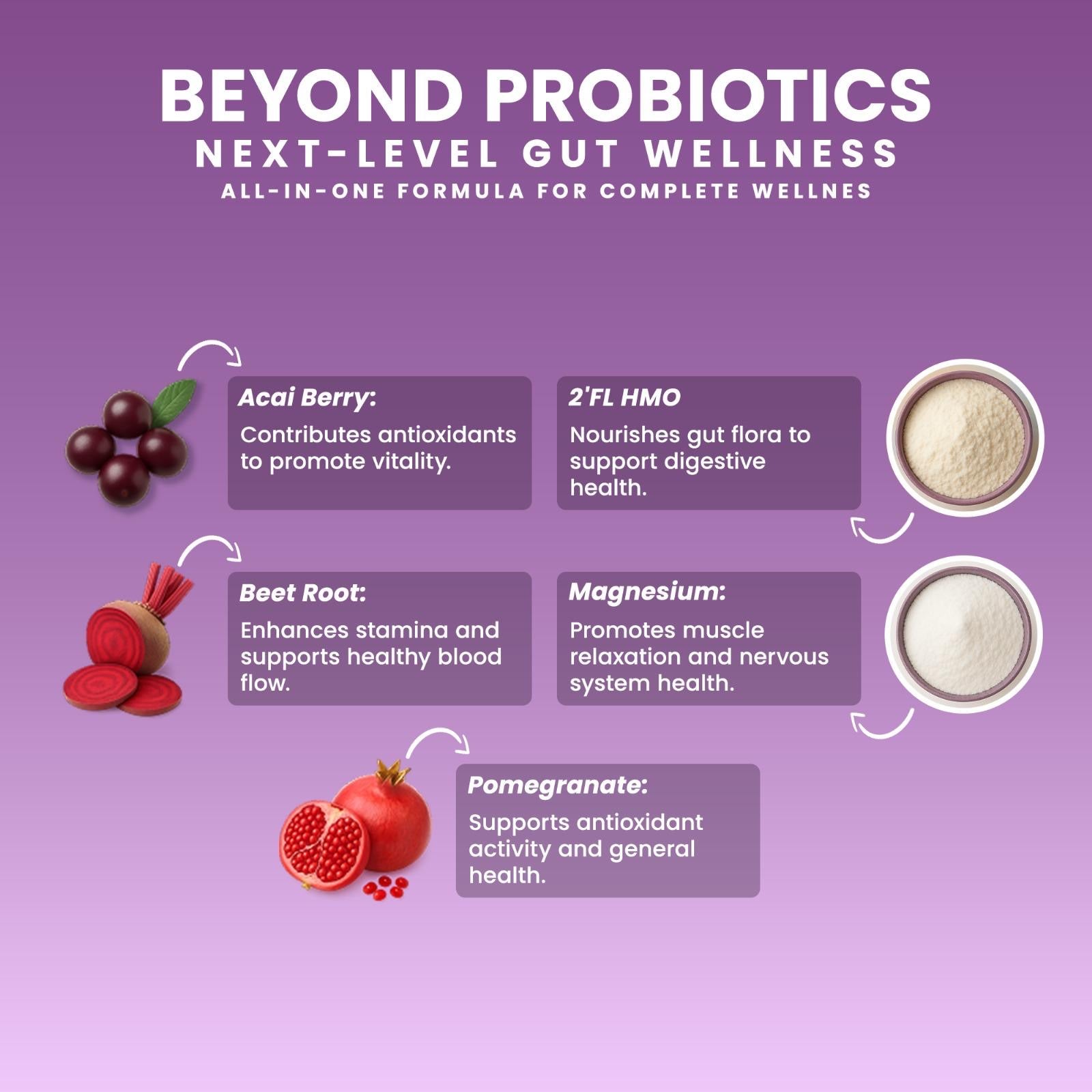
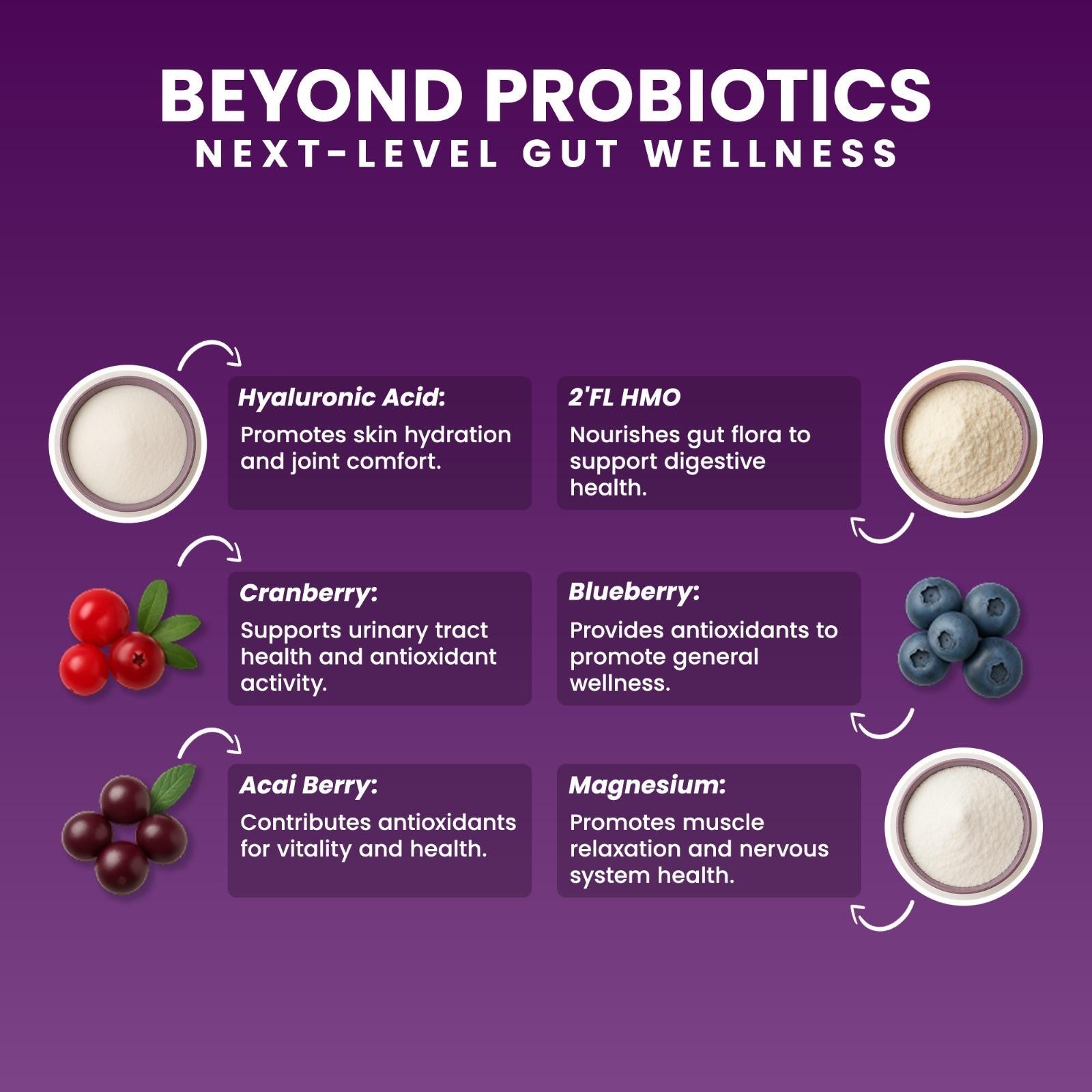
1. Eat Polyphenol-Rich Foods
Berries, cocoa, pomegranate, and green tea all support beneficial bacteria.
📚 Dietary Polyphenols & Gut Microbiota — Wang et al., 2022
👉 https://pmc.ncbi.nlm.nih.gov/articles/PMC9220293/
2. Add Prebiotics
(Inulin, FOS, resistant starch)
Prebiotics feed beneficial bacteria and improve SCFA production.
3. Support HMOs (Especially 2’-FL)
HMOs nourish mucosal bacteria and strengthen the gut barrier.
📚 HMO 2’-FL Supports Gut Barrier — AJCN
https://pmc.ncbi.nlm.nih.gov/articles/PMC6164445/
4. Use SCFA-Supportive Probiotics (Clostridium butyricum)
These support epithelial repair and intestinal resilience.
📚 C. butyricum Supports SCFAs and Mucin — PMC
https://pmc.ncbi.nlm.nih.gov/articles/PMC8078720/
5. Use Chewable Microbiome Formulas
They support both the oral and gut microbiome — offering a dual-pathway advantage that capsules cannot.
Akkermansia: A Keystone Microbe in the Human Microbiome
Akkermansia muciniphila is essential for:
-
mucin regeneration
-
gut barrier strength
-
inflammation control
-
metabolic balance
Learn more:
👉 Akkermansia: The Missing Microbe for Gut Health, Oral–Gut Balance & Digestive Strength
https://akkermansia.life/blogs/blog/akkermansia-the-missing-microbe-for-gut-health-oral-gut-balance-digestive-strength
🟦 INTERNAL LINKS
👉 What Is the Human Microbiome? A Complete Guide to Microbes, Immunity & Digestion
👉 Oral Microbiota & Gut Health: How the Mouth Shapes the Entire Microbiome
👉 The Gut–Brain Axis: How Microbes Influence Mood, Stress & Appetite
👉 Microbiome Development From Birth to Adulthood
✍️ Written by Ali Rıza Akın
Microbiome Scientist, Author & Founder of Next-Microbiome
Ali Rıza Akın is a microbiome scientist with nearly 30 years of biotechnology and translational research experience in Silicon Valley. He is the discoverer of Christensenella californii, a novel human-associated bacterial species linked to metabolic health and mucosal integrity.
His scientific work spans:
-
mucosal immunology
-
gut barrier biology
-
oral–gut microbiome interactions
-
SCFA metabolism
-
next-generation probiotics (Akkermansia, Christensenella, Clostridium butyricum)
-
host–microbe signaling
-
microbial therapeutics
He is the author of Bakterin Kadar Yaşa: İçimizdeki Evren (Live as Long as Your Bacteria) and a contributor to Bacterial Therapy of Cancer: Methods and Protocols (Springer, Methods in Molecular Biology).
As Founder of Next-Microbiome, Ali develops advanced synbiotic formulations — including the industry’s first chewable Akkermansia-supporting synbiotic — designed to strengthen the gut lining, support metabolic resilience, enhance mucosal immunity, and harmonize the oral–gut microbiome axis.